proximal tibiofibular joint dislocation

Clinical Presentation
Isolated PTFJ dislocations are rare, accounting for less than 1% of all knee injuries. Once dislocated, the fibular head sits in an anterolateral position, with the anterior surface of the superior tibia directly behind.
The mechanism most commonly follows a fall with the following anatomical positions occurring at the point of dislocation – ankle inversion, foot plantar flexed, and knee flexed or hyper-flexed
A tender deformity appears at the proximal fibula area, the knee usually held in full extension.

Technique
Click below for a clinical demonstration of the technique being performed on a patient. At the bottom of this page is a case report and review article with additional detail on the technique and underlying anatomy (with thanks to my co-authors Nick and Jake!)

Imaging
A number of case studies have demonstrated the risks of misdiagnosis with unilateral lower limb imaging so do bilateral knee imaging to allow direct comparison.
CT may be needed in cases with inconclusive x-ray findings and those of suspected fractures.
Proximal tibio-fibular joint dislocation

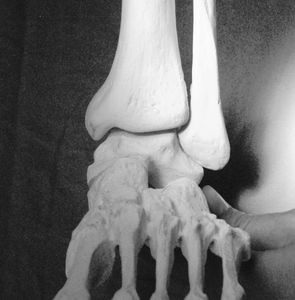
Anatomy in dislocation
Once dislocated, the fibular head sits in an anterolateral position, with the anterior surface of the superior tibia directly behind. From this position, the head must travel inferiorly, laterally, posteriorly and then medially in order to reduce.
Obstacles to reduction
- The flared lateral aspect of the superior tibia, which provides a bony posterior obstacle. This posterior obstacle is reduced inferiorly due to the shape of the tibia.
- Tension of the lateral collateral ligament and biceps femoris tendon. These stop the descent of the fibular head, and pull the head superiorly and against the anterior surface of the tibia.
- The ankle is no longer in an exaggerated inversion/plantar flexion, so the ability of the distal fibula to move inferiorly is impeded.
- The knee is no longer flexed, resulting in further lateral collateral ligament tension.

Step-by-step technique
Sedate patient
Place ankle into inversion and plantar flexion
Flex knee to 90 degrees
Apply downward pressure to the fibular head, which can then be guided laterally and posteriorly if required
What's up Nick?

Necessity is the mother of creation!
I’d never seen a proximal fibula dislocation until Nick Farebrother @Apostalidis came through to the main area of the emergency department and said “come and see this guy, I think he’s dislocated his fibula!” Nick is one of our nurse practitioners and very much a gun where it comes to musculoskeletal pathology so had already organised for bilateral X-rays to confirm his suspicion, and done a background search on the injury. There wasn’t a reduction technique so I worked out the dislocation anatomy and came up with a plan by the time the patient was back from X-Ray. This is why I love emergency medicine, just when you think you’ve seen everything, an unusual case will come through the door that forces you to be creative and problem solve in real time!
review article: isolated PTFJ dislocation






The Sartorial technique – an auto-reduction method for PTFJ
Recurrent PTFJ dislocation
After posting the video of the PTFJ reduction technique, there was a lot of comments from people who have had this injury occur repeatedly with minor trauma, specific positions, or spontaneously.
Mechanisms include:
- sitting cross legged on the floor with legs bent +/- soles of feet facing each other. This can be seen with “tailor sitting” which is sometimes recommended for posture in pregnancy, “criss cross apple-sauce” as a recommendation for kids sitting cross-legged at school, and badhakonasana pose in yoga.
- squats especially performing weighted knee split squats, pistol (single leg) or variants such as dragon, shrimp or pistol with overhead press.
kneeling with knees apart and ankles inverted.
Tailor sitting

Sitting cross legged, sometimes recommended for posture and back pain in pregnancy.
https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=zm6021&lang=en-ca
badhakonasana

This yoga pose also known as the butterfly pose combines knee hyperflexion and ankle inversion. Leaning forwards can also add more weight into the knee.
Pistol squats

Join our community of fitness enthusiasts and enjoy our wide range of group fitness classes. From yoga to spin to high-intensity interval training, we have something for everyone. Get fit, have fun, and make new friends!
Pistol with overhead press

Pistols with overhead press, dragon squats, shrimp squats, or even simple weighted split squats can be built up to and performed safely. But a stumble or malaligned knee when performing them may expose the knee to unusually transmitted forces.
https://www.crossfit.com/essentials/gymnailing-it-pistols-and-overhead-squats
Mechanism of injury
These positions combine the noted mechanism of injury combination of ankle inversion, foot plantar flexed, and knee flexed/hyper-flexed. Hypermobility syndromes such as Ehler’s-Danlos syndrome may be a compounding factor. I thought it would be useful for people who have this occur atraumatically or positionally to have an auto-reduction technique that they can use to quickly reduce their own proximal fibula dislocation. I call it the sartorial technique.
The sartorial technique - an auto-reduction method for PTFJ

Technique description
Step 1 – Sartorial position. Seated on chair with hip and knee bent, and foot resting on the opposite knee.
Step 2 – Ankle moved into full inversion.
Step 3 – Fibula head pushed inferiorly (down towards foot).
This technique uses the principle of positioning the dislocated fibula back into the position of weakness and then specifically moving the whole fibula bone inferiorly to roll the head past the flared tibia which it has been locked behind. It requires the person to be able to bend their knee enough to place their foot on the opposite knee as shown, and also to have intact lateral ligaments in the ankle of the affected limb – these are required for step 2 to pull the fibula inferiorly. The fibula may reduce with each of the manoeuvres that progressively move the fibula head into a position favouring reduction.

Why call it the sartorial technique?
Sartorius is one of my favourite muscles in the body. As well as being the longest muscle in your body, it is named after the position that tailors (latin – sartor) sit in while working. When flexed the sartorius bends the knees and hips and rotates the femur (thigh bone) outwards. This gives you the starting position for this technique.

Thanks for the feedback!

Joe Lauden's knee
As mentioned above, the idea for this technique came from a number of posts under my PTFJ YouTube video from people who were describing this type of injury occurring to them. One of them mentioned a UFC fighter called Joe Lauden who had to cancel a fight due to a knee injury. This may have been a PTFJ, without examining or imaging the knee it's impossible to say.

Ben Patrick's knee
Joe had seen one of Ben Patrick's videos (link below) where Ben discusses having a similar recurring injury which usually popped in . The one time it didn't he intuitively tried putting it in the same position that it popped out in . You can see this approach in many types of dislocation techniques. Hopefully, the above technique and description explains the anatomy underlying this, and adding in the deliberate inversion and fibula head manipulation should work well for this type of injury. Ben (aka kneesovertoesguy) also does some interesting stuff with floss tape, worth a watch. Nice work, Ben!
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.