Which shoulders should I image before reducing?

Which cases are safe to not X-Ray?
Anterior dislocations with Bankart’s or Hill-Sach’s lesions, greater tuberosity avulsion fractures are all suitable for closed reduction. Only imaging will be able to definitively confirm or deny this. However, if your patient has a combination of a clear history of injury (pulling motion in or forced abduction/elevation in zero position), with a clear clinical examination (acromial step, palpable humeral head, intact AC joint, absence of bruising to upper arm) then you should be safe to attempt a technique that does not use traction, forced leveraging or torsion. Always with the proviso that you are ready to fail – declare that you will stop if it is painful for the patient. I’ll happily place someone into the analgesic position 1 and then use a Cunningham technique even if strongly suspect a GT# as I’m not using any traction or torsion – I just won’t move to another technique if reduction doesn’t occur immediately or if the patient is unexpectedly uncomfortable or unable to relax.
For more on ‘preparing to fail’ and an algorithmic technique click below.

Could there be a shaft fracture?
Definitely image if there is any chance of a humeral shaft fracture. If your patient has fallen directly onto the shoulder, is elderly or at some other risk of osteoporosis/pathological fracture, then I would want to exclude a humeral shaft fracture prior to any manipulation. Neurological deficit (usually axillary nerve injury) would also require an X-Ray.
Excessive pain or inability to move towards a position of comfort would also trigger an X-Ray. Finding a comminuted fracture can be really useful information especially if you have the rare experience of hitting a barrier during a zero position technique – you may have an obstructing fragment. Solution – move to a scapular manipulation technique to get the fragment out of the path of the reducing head.

What is the significance of a greater tuberosity fracture?
Not every greater tuberosity fracture is the same. An avulsed GT fragment (top picture) has a different mechanism (pull) to a comminuted fracture (impact) and the risk of an underlying fracture line is infinitely higher with the latter type. Turning a humeral neck fracture from undisplaced to displaced with your attempted manipulation is definitely one to avoid. There is a great case example published by Jung Ho Park in which a 74-year old man fell from a motorbike and landed on his left shoulder (impact mechanism). If you look at the initial films (above pics) the GT is not very displaced but is definitely comminuted – mechanism and GT# type now both suggest impact with risk of underlying humeral neck #. Traction/counter-traction technique had predictable results, but even using a gentle zero position may have had the same effect.
Take home message – if your patient is at higher risk of underlying pathological fracture, has an impact mechanism, or an impact fracture pattern of GT then CT to exclude an undisplaced proximal humeral fracture before you manipulate.
What is a Bankart's lesion?
What is a Bankart's lesion?
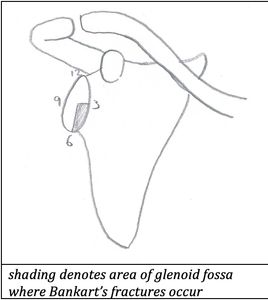
Classically the Bankart’s lesion is described as separation of the joint capsule and/or labrum from the anteroinferior glenoid rim, however the term is commonly used to refer to bony disruption of the glenoid – the bony Bankart’s lesion or Bankart’s fracture. This fracture occurs in approximately 22% of anterior dislocations and is the result of impaction of the humeral head against the antero-inferior glenoid labrum during dislocation, and is associated with rupture of the joint capsule and inferior gleno-humeral ligament damage. This is usually seen as a subtle lucent line in the antero-inferior ‘3-6 o’clock’ area of the glenoid with an adjacent fracture fragment.

The presence of a classic Bankart’s lesion cannot be determined from plain X-rays. A CT (computed tomography) scan of the shoulder can be performed to determine the origin of bone fragments. An MRI is the best scan to delineate the extent of a Bankart’s lesion.
What is a Hill-Sach's lesion

What is a Hill-Sach's lesion?
A Hill-Sach’s lesion is an impact fracture causing a depression of the postero-lateral aspect of the humeral head occurring during anterior dislocation. This injury has been reported in 54-76% of cases of anterior shoulder dislocation.

What is a reverse Hill-Sach's lesion?
Also called a McLaughlin lesion, this is a depression of the anterograde-medial aspect of the humeral head occurring during posterior dislocation.
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.